By: Erin Beck, Staff Writer | Posted: Jan. 20, 2018 | Source: WV Gazette-Mail
When you first started seeing your doctor, did people say how much you paid would be based on how much you could afford? Do people at the doctor’s office help patients find transportation to appointments?
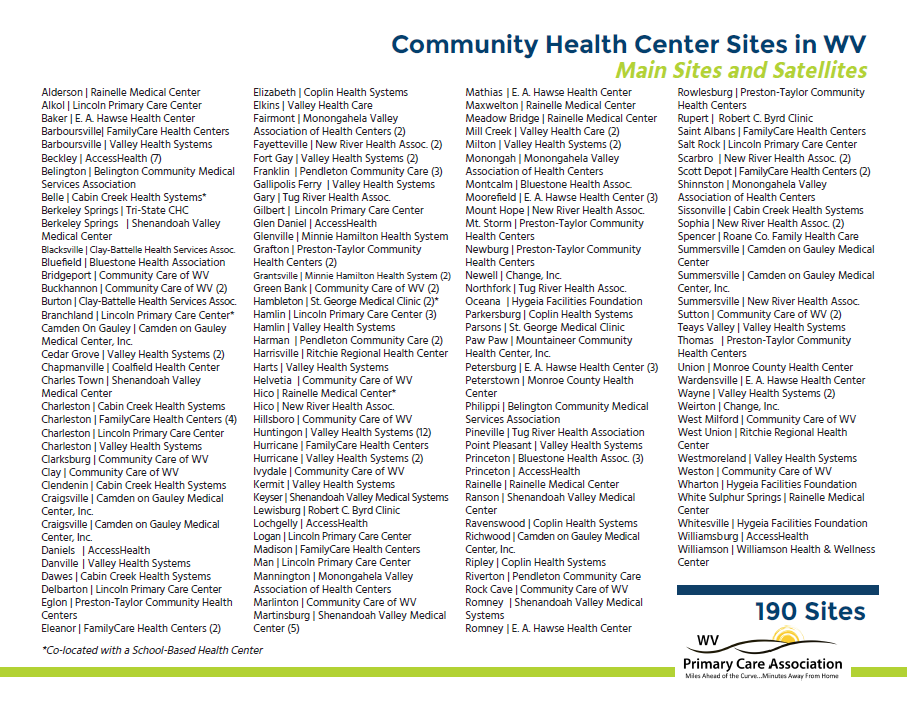
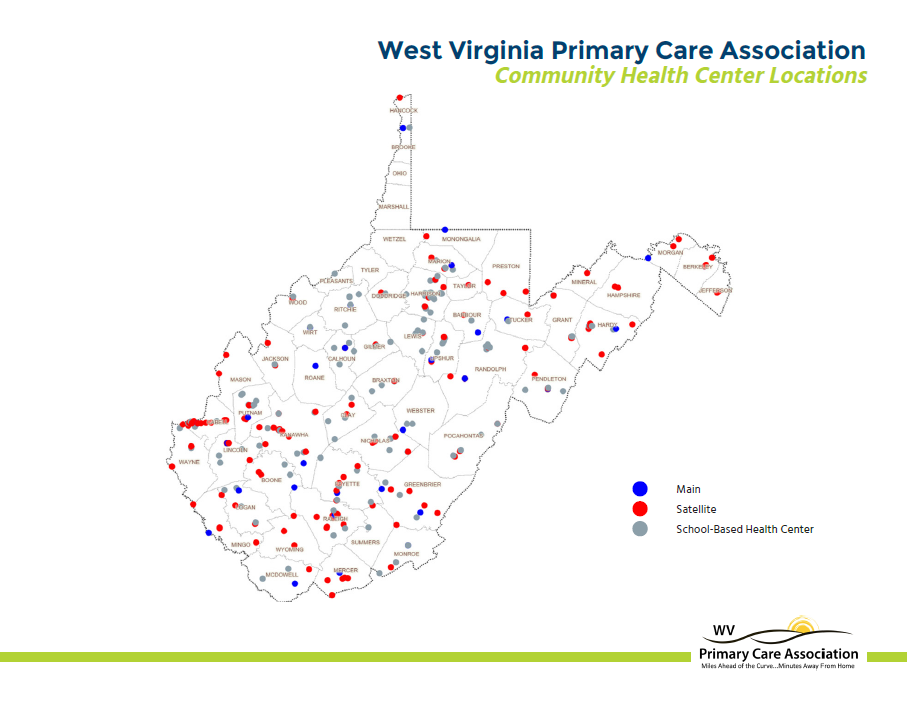
Chances are, you go to one of the 300 locations of 31 federally qualified community health centers in West Virginia. About one in four West Virginians do, according to the West Virginia Primary Care Association, compared to about 8 percent of people nationwide.
Locations include many of the school-based health centers that have opened in West Virginia in recent years and centers that employ the only primary care providers — such as a family doctor — for miles.
The centers are called “federally qualified” because they’ve agreed to offer a range of health care services — such as pediatrics, women’s health, dental and preventative services, like flu shots — and give discounts in areas where health care is hard to come by in exchange for grant money from the federal government.
Congress let that grant funding — $3.6 billion in federal fiscal year 2017 — expire Oct. 1. Funding for the Children’s Health Insurance Program, which covers 9 million children, expired at the same time.
Advocates for CHIP have complained that, after the GOP-led Congress finished extensive debate on several bills to repeal the Affordable Care Act, they turned to negotiations on a bill that cut taxes for corporations instead of funding CHIP.
 In an interview last week, leaders of several federally qualified health centers in West Virginia noted they, too, have been waiting.
In an interview last week, leaders of several federally qualified health centers in West Virginia noted they, too, have been waiting.
Cabin Creek Health Systems has locations in Cabin Creek, Kanawha City, Riverside High School, Sissonville and Clendenin. Its location in Clendenin closed for several weeks after the June 2016 flood. An AmeriCorps VISTA volunteer worked in the once-flooded basement to link flood victims with services.
Dr. Mitch Jacques, medical director for Cabin Creek, noted that he doesn’t typically talk to reporters.
“My wife told me once when I was involved in this a few months ago that if I didn’t speak up for the people I cared for, no one else would because they can’t speak for themselves, and I think that’s very correct,” he said. “They’re segments of our population who don’t get heard in Washington because they — and I won’t say why, but our patients, in many cases, worked all their lives. They’re down and out now, or they’re living in a rural area and isolated. But they don’t — our congressional voices don’t always hear their voices loudly enough in terms of what they need.”
He took a long pause.
“It breaks my heart,” he said. “I don’t know any other way to say it.”
The Milken Institute School of Public Health at The George Washington University and the RCHN Community Health Foundation, which was established to support community health centers, estimated the funding loss would mean 76,000 to 161,000 jobs lost nationwide and 654 to 1,398 jobs lost in West Virginia.
The lower number is based on the elimination of the $3.6 billion grant, while the higher number assumes community health centers would have difficulty serving insured patients, so they would lose Medicaid and other insurance money.
“In rural areas, they’re some of the best jobs there are,” Jacques said.
Dr. Matt Weimer, director of quality at Valley Health Systems, based in Huntington, said the uncertainty has made it hard to recruit and retain employees.
“Obviously, at the end of the day, that all impacts patient care,” he said.
Community health centers serve a wide range of people, including those who can’t pay for care and those who don’t live near other health care providers.
Others choose the centers for the quality of care. The centers use a team approach to care for the whole person — maybe that means your primary care provider helps you with your hypertension, then links you with the addiction treatment program, or a medical assistant helps you shower.
No one is turned away.
“I’m a health center patient,” said Martha Carter, CEO of FamilyCare Health Centers. “I get good care that I don’t know I would get other places.”
The federal government partially shut down early Saturday. Nearly four months after funding for both CHIP and community health centers expired, the U.S. House of Representatives agreed on a funding bill earlier this week that included six-year CHIP funding but no money for community health centers. The Senate failed to reach an agreement.
Carter said the loss of the grant would equal a $2 million loss for her center. FamilyCare has locations in Charleston, St. Albans, Eleanor, Hurricane, Barboursville and Scott Depot, according to its website.
“We’d like to expand our addiction services, our substance abuse treatment services, but any program that is in a startup phase requires capital and requires some time before it’s self-supporting, and that’s not a risk that we can take right now,” she said. “We’ve had some opportunities for new sites that I can’t even think about investing in right now because I don’t know that I can support what I currently have, let alone expand to new sites.”
“If our program isn’t going to get funded, where should we cut?” she added. “Should we start with behavioral health? With substance abuse? With dental care? Tell us where we should cut.”
Community health center leaders said those programs would likely be cut first. West Virginia has the highest drug overdose death rate in the country; the highest rate of severe mental illness, according to a national 2012-2014 survey from the Substance Abuse and Mental Health Services Administration; and fewer dentists than most other states, according to the American Dental Association.
Amy Simmons Farber, a spokeswoman for the National Association of Community Health Centers, said health centers were given a “small percentage of normal funding” during an earlier short-term spending bill, but centers still face “a funding cliff.”
Louise Reese, CEO of the West Virginia Primary Care Association, said U.S. Sens. Joe Manchin, D-W.Va., and Shelley Moore Capito, R-W.Va., have verbally expressed support, but Congress is “riddled with dysfunction.” They’ve been told they were “next on the list,” she said.
“Tell us which program doesn’t matter,” she added.
Reach Erin Beck at 304-348-5163, erin.beck@wvgazettemail.com,
Facebook.com/erinbeckwv or follow
@erinbeckwv on Twitter.